Anorectal abscess
Anorectal abscess signifies inflammation of the fat in one of the spaces surrounding the anorectum.
Infections from rectum by anal glands, which are situated in anal crypts of the anal canal, penetrate perianal tissue. Crypt abscess always is at the level of the dentate line. The reasons of crypt abscess are different: constipation, hemorrhoids, anal fissure ecc.
Anal gland infection is also the principal cause of anal fistulas. Classification of anorectal abscess is based on involved fat space. There are perianal abscess, ischiorectal abscess, supralevator abscess, postanal abscess, horseshoe abscess (anterior and posterior).
Clinical feature of anorectal abscess
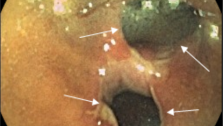
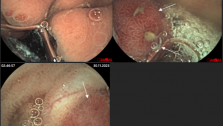
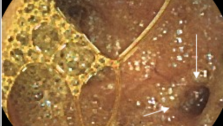
There are cardinal clinical signs of anorectal abscess: swelling, redness, pain of perianal region, difficulty in sitting, walking and painful defecation (not always). Fluctuation in the center of redness can also occur. Subsequently, patient’s condition worsen, they get fever, especially, in deep abscess case (ischiorectal, supralevator abscesses). In some cases (superficial localization) patients condition doesn’t change. Abscess localization and internal opening are identified by digital examination, anoscopy, rectosropy, intrarectal ultrasound examination, dyestuff test.
Inspection of perianal area allows to fine local symptoms (redness, swelling, local warmth). Next examination is digital (important for deep abscesses). Next step is puncture and painting over the abscess that allows identifying internal opening.
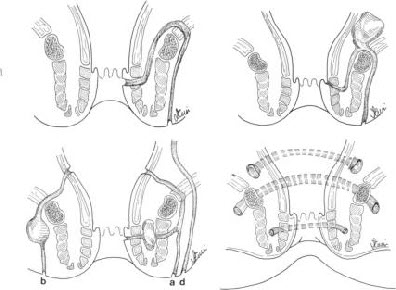
Anorectal abscess is treated only by operation. There are two types of operations: radical (with primary fistulotomy) and symptomatic (incision and drainage without fistulotomy). Radical operation is possible only in proctology department.
In surgical department perianal abscesses usually are managed symptomatically and after this treatment patients have quite high risk of development persistent fistula. Surgical treatment also can be performed in one phase (with primary fistulotomy) and in two phases (if fistula can not be identified right away, first surgeon realizes incision and drainage and in several days he detects fistula and makes fistulotomy).
If abscess bursts itself or is inserted by surgeon (without fistulotomy) usually anal in some period anal fistula appears. Internal opening in anal canal doesn’t heal over and there is the reason of chronic anal fissure (70% of clinical cases of anorectal abscess). External opening can appear in other area. Infection persists because of high-virulent microorganisms, which come through internal opening from rectum. In this case some period after incision patients feel well (without any discomfort).
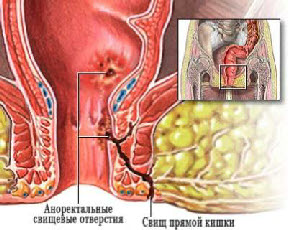
There are two types of fistula:
- Complete anal fistula (such fistula has internal opening, which is localized in one of the anal crypts, and external opening in perianal area)
- Incomplete anal fistula (which has only internal opening) Fistulas also can be simple and difficult. Scar tissue in crypt’s area, two and more external openings, presence of abscesses is the features of difficult fistula.
Defining the trajectory of the fistula in relation to the external sphincter establishes to the following classification
- Intershincteric fistula
- Trans-sphincteric fistula (which passes throw through the external sphincter)
- Suprasphincteric fistula is the most difficult and passes out of external sphincter
Intershincteric fistula is the simplest type of fistula. Usually, the trajectory of such fistula is straight, and scar tissue is not manifest. The disease is not long standing. The external opening is close to the anal verge. Internal openings can be located at any of anal glands, on dentate line level.

Trans-sphincteric fistula is more common than extrasphincteric but can be low and high (can passes through deep, subcutaneous or superficial part of external sphincter).
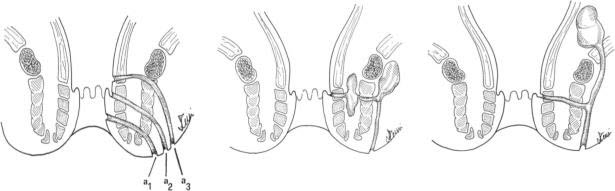
Suprasphincteric fistula can be different complexity.
The first level of complexity means that fistula has small internal opening without scar, abscesses or indurations in fat and its trajectory is quite straight.
The second level of complexity means that scar around I nternal opening is evident but patient has no abscess or indurations in fat.
The third level of complexity. Internal opening is small, without scar, but there are some abscesses or indurations in fat.
The forth level of complexity. Internal opening is large, with scar around, there are some abscesses or indurations in fat.
Clinical features of anal fistula
Clinical features of anal fistula. Usually, patients with anal fistula have some discomfort in perianal area. First of all, because of wound (external opening) in the skin close to anus and also because of pus or blood outflows from this wound. Patients have to wash this region very often or makes sits bath. Sometimes they have itch. Patients rarely have any pain that is typical only for incomplete anal fistula (pain increases during defecation and slowly increases in several minutes).
Patients feel quite well up to next abscesses (which appears in some weeks month or even years). If perianal abscess again is managed by incision and drainage without fistulotomy patient feels well in some days, but wound in perianal skin (smaller than 1cm) doesn’t heal over completely. There is external opening with permanent pus outflow. Sometimes patient can see blood that is draining from this wound. It can be the sign of malignant fistula.
In periods of remission the pain is not characteristic feature of anal fistula. Patient is in satisfactory condition. If patient to use hygienic procedures thoroughly, he can not so suffer from anal fistula for a long time. Appearance of new focuses of inflammation, drawing external sphincter into this process is a cause of new symptoms of disease appear: headache, sleep disturbance, performance decrement, low sexual potency, mental disturbance.
Complications of anal fistula
1. Fecal incontinence, due to difficult local changes with deformation of anal canal and perineum, scar process in muscular tissue of external sphincter.
2. Anal stricture of anal canal, due to scar laxity.
3. Malignant fistula (usually when fistula exists more than 5 years)
Diagnosis of anal fistula
Diagnosis of anal fistula is based on typical examinations: inspection of perianal area (there is wound in skin close to anus), digital examination (is necessary to fine internal opening). Other examinations (probe, examination with brilliant green solution, intrarectal ultrasound) are necessary to identify the type of fistula.
Differential diagnosis of anal fistula includes Crohn’s disease, pilonidal sinus, tuberculosis, actinimycosis.
Read also Treatment of anal fistula